7 things Nevada is doing to fight the opioid abuse epidemic

It was Michael Yenick’s love for the community, his desire to be a “hometown hero,” that prompted him to choose the University of Nevada, Reno over the other schools that were recruiting him to play football, his mother says.
It was the hard hits from playing defensive end, the back injury and the two knee surgeries and the painkillers that a hometown doctor prescribed him, that led to his downfall. In October 2015, he died of an opioid overdose at the age of 33, and his parents have been fighting ever since to prevent more young people from losing the same battle.
“He would want us to do that,” his mother, Cyndi, told attendees at the Governor’s Opioid State Action Accountability Task Force on Monday.
Gov. Brian Sandoval and his wife Kathleen have been active over the past few years trying to fight opioid abuse, which is a primary driver behind the 619 drug overdose deaths the CDC counted in Nevada in 2015. The state has one of the highest rates of opioid painkiller prescription in the country, with 87.5 prescriptions per 100 state residents in 2016 compared with 66.5 per 100 nationally, and hospitalizations where opioid abuse is a contributing factor have more than doubled over the past six years.
But the dramatic case of an illegal prescription drug ring in Reno, which has been linked to Yenick’s death, particularly moved the governor, according to his chief of staff. Sandoval convened a prescription drug abuse summit in the summer of 2016 that drew about 500 people and led to a detailed plan to address the crisis, and at one point set a goal of reducing abuse by 18 percent by 2018.
He’s now having the task force meet periodically to offer updates on progress.
“I don’t have the words to tell you how sorry I am in what you have gone through,” Sandoval told Yenick’s mother during the meeting. “But I will tell you ... that that has been an inspiration and a motivator for me to get this done because it’s inconceivable to me what you’ve been through.”
Sandoval’s office has also spearheaded two major bills over the last two sessions that seek to get a handle on the crisis. Among the strongest supporters in the Legislature is Sen. Patricia Farley, who is in the process of being certified as a foster parent so she can take four nieces and nephews into her home next month. Their parents became addicted to drugs and lost custody.

“It was a dirty secret we didn’t talk about,” Farley said about the opioid addiction issues in her family following a Wednesday news conference on the issue. “We didn’t have the resources and we didn’t know where to go to get help. What you had is a bunch of people who’d never really seen it before trying to deal with it.”
She said she hopes the state can do more to educate youth and stave off future addiction, but also provide the mental health and wraparound services that addicts need during a recovery process that can last a lifetime.
Here are seven things the state is doing to fight the epidemic:
1. BETTER TRACKING OF OVERDOSES
Ask whether Nevada’s opioid problem is improving and you might not get a clear answer.
“Although it’s difficult to provide a general response to the question, the Department of Health and Human Services and the Division of Public and Behavioral Health have seen some improvements,” state officials told The Nevada Independent. “We see mortality rates decreasing and we see that overdose hospitalizations have not increased over the past seven years, which is a positive.”
It’s true that poisonings — what most people would understand as an overdose — have remained mostly flat, with the 576 inpatient cases in 2016 just a slight change from 599 cases in 2010. And the rate of opioid-related deaths has dropped from 16.9 per 100,000 in 2011 to 13.3 in 2016.

But hospitalizations where medical personnel indicate the patient is abusing opioids or dependent on the drugs are veering upward. There were 3,899 such inpatient cases in 2010 and 8,210 in 2016.
“There isn’t a clean check box on any inpatient admission forms that say yes, this is an overdose. There are a lot of things that a provider in the ER could look at to consider something an opioid overdose,” said Elyse Monroy, Sandoval’s health and human services policy analyst. “We know that deaths have gone down. We don’t really have a good, complete data picture to say we know why.”
The state wants to get a better handle on where its problem areas are — both geographically and otherwise. A new law passed this spring requires health-care providers to report to the state whenever they encounter an overdose or suspected overdose case. That kind of reporting was previously only required of certain contagious diseases.
“We will have more real time reporting of opioid overdoses from the facilities which may serve as a surveillance system to monitor opioid related overdoses more timely and accurately,” the health department said.
The data it currently keeps is being distributed to service and treatment providers, work groups trying to study and address the problem, and to inform state grant writing efforts.
State statisticians are working to develop online “dashboards” that update frequently and let the public explore opioid abuse trends and hotspots down to individual ZIP codes. State statisticians told the panel that they hope the dashboards would be ready for a review by the next time the panel meets, in January.
The data are limited based on the quality of the input, and it’s not always cut-and-dried. For example, the state maintains statistics on how many times first responders administer naloxone, which can reverse the effects of an overdose.
But it’s categorized by the number of calls to emergency services reporting an overdose; sometimes, a single overdose can lead to multiple calls. State statisticians told the panel they weren’t sure where to begin on how to correct the data and reflect multiple calls on single overdoses.
2. DISTRIBUTING NALOXONE
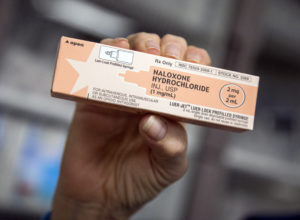
Nevada greatly increased access to naloxone, a drug that can quickly reverse the toxic effects of an opiate and prevent an overdose, during the 2015 legislative session. While state law in the past allowed practitioners to prescribe the drug to people at risk of experiencing an overdose, the so-called “Good Samaritan Drug Overdose Act” made such prescriptions available to family members, friends and other people who might be around when a person overdoses, including emergency medical technicians (EMTs).
An effort called the Nevada Rural Opioid Overdose Reversal project (NROOR), which brought together UNR, rural hospitals and state emergency personnel, trained 117 EMTs last year to recognize the effects of an overdose and respond with naloxone. A $100,000 grant from the Federal Office of Rural Health Policy helped them purchase 500 pre-filled syringes of naloxone — a drug that costs about $75 for two doses — and distributed them to EMTs in seven rural counties.
But with most of the doses set to expire in November, rural EMTs have administered only five of them. Program administrators had projected the number of doses based on hospital billing data, emergency room admissions and overdose deaths.
“The data that we have so far suggest these EMTs are not necessarily being called to overdose emergencies with the frequency we expected,” said Karla Wagner, a UNR professor who’s evaluating the partnership’s success.
Wagner said it’s possible people aren’t calling 911 after a friend or family overdoses and are taking the person to the ER themselves, perhaps because they fear they’ll get in trouble for drug use. She said it shows a need to educate the public about the Good Samaritan law that gives some criminal immunity to people who report an overdose.
The program plans to redistribute the unused naloxone to community health centers in more populous areas, including Trac B in Las Vegas and Nevada Hopes in Reno, so they might be used before they expire.
The agency said it’s hoping for better data so naloxone can be targeted more efficiently in the future. The grant was a one-shot award and the partnership is seeking ways to remain sustainable.
One obvious success, though, was that the initiative appears to be boosting overdose knowledge among first responders. Only 18 percent knew who could legally possess the drug before the training, and 50 percent of participants correctly answered the question afterward.
Aside from the rural EMTs project, naloxone is available elsewhere. A survey sent to nearly 400 Nevada pharmacies found that 80 percent of respondents stocked naloxone, and there were 660 doses furnished by pharmacists since the 2015 law passed — all of which could potentially save a life.
3. MAKING TREATMENT EASIER TO FIND

State officials acknowledge they don’t have enough treatment providers to handle the demand, but they landed a $6.5 million federal State Targeted Response grant from the Substance Abuse and Mental Health Services Administration that they hope can grow capacity and quickly connect people to the appropriate services.
Nevada is building up a “hub and spoke” model similar to one used in Vermont so there’s no wrong door when patients go seeking help for an opioid problem.
“One of the issues we’ve realized in our state is the lack of connectivity to services,” said Dr. Stephanie Woodard, who’s overseeing the project. “There’s really a lack of knowledge about how they would get someone into treatment if they encountered a patient needing treatment.”
The state issued a request for applications last week for clinics that want to be one of at least three “hubs” in the state, called “Integrated Opioid Treatment and Recovery Centers.” Those centers will offer a range of medical services such as psychiatry and the ability to do medical and behavioral health screenings.
They’ll have formal written agreements with agencies that provide services such as transitional housing, methadone treatments and HIV/hepatitis C testing. The “hub” will guide people to the appropriate agency to continue treatment — those agencies are the “spokes” in the model.
While insurance, including Medicaid, would pay for much of the direct cost of services, the grant money will help clinics ramp up their services, upgrade their electronic health records and “onboard” new staff.
“These grants are very finite. We need to be very smart about how we use these dollars,” Woodard said. “I don’t want to build a system that is dependent on dollars only to know in two years they’re going to go away.”
As for Medicaid itself? Groups including the Children's Advocacy Alliance praise Sandoval's decision to expand coverage, which means nearly 9,000 more opioid addicts in Nevada have insurance and can access treatment such as medication that reduces cravings and withdrawals.
4. FLAGGING OVER-PRESCRIBERS

Sandoval backed bills in 2015 and then again in 2017 that seek to put a check on the pace at which doctors are prescribing and ensure accountability for unnecessary prescriptions. The first bill, SB459, required prescribers to check the state’s Prescription Monitoring Program database and review a patient’s prescription history before calling for more opioids.
The database, which has been around since 1997, was meant to curb “doctor-shopping” — when patients go from doctor to doctor hoping a different person will write them an additional prescription. While the number of providers enrolled has jumped from 16 percent to 81 percent in recent years, the state hopes to close the gap.
AB474, passed in 2017, requires all providers to enroll in the Prescription Monitoring Program and makes it easier for boards to use the system to address over-prescribing — an issue that had previously drawn few complaints and was a low investigative priority for the boards that oversee medical professionals.
Monroy said that in the past, occupational licensing boards might receive notification that a doctor was writing a large number of prescriptions, but they often didn’t act upon the notice because doing so would constitute a full-fledged investigation. Under the new legislation, boards must follow up on the notifications but under the less draconian “administrative review” process — which can be used as an opportunity to educate a provider or gather more information and doesn’t necessarily escalate to the level of an investigation.
The new bill, which takes effect Jan. 1, 2018, requires providers to take two hours of continuing education on drug abuse issues and go through a list of steps before issuing an opioid prescription. Those include having a bona fide relationship with the patient, doing a risk assessment on them, creating a treatment plan and obtaining their written consent.
The detailed guidance, which varies based on the length of the prescription, is an expansion for a state that had previously only used federal Centers for Disease Control and Prevention guidelines and didn’t have state-level mandates. It also ensures more frequent use of the prescription monitoring database, requiring prescribers to check for a patient in the database every 90 days rather than just when an initial prescription is written.
Boards are now drafting regulations based on the bill that will address topics such as how to discipline for over-prescribers.
The Nevada State Board of Medical Examiners, which has about 7,000 licensees who can prescribe, said it now has a dedicated attorney, investigator and a staffer focused exclusively on prescribing cases.
5. TAKING BACK DRUGS

In the past eight years, efforts to round up unused pills and prevent them from ending up in the hands of youth or other potential addicts have gained steam.
The first Washoe County drug roundup in 2009 netted 39,471 pills, while that number was nearly five-fold — 224,416 pills — in the April 2017 roundup. Clark County counts their collections in pounds and not pills, but they rounded up 1,052 pounds in an April takeback.
With help from coalitions that are fighting drug abuse, all counties are collecting prescription drugs through drop boxes or designated takeback days. They’re also taking additional steps to help people keep tabs on and quickly dispose of their drugs, including passing out drug tracking cards and Deterra bags, which deactivate pills and offer a safe way to dispose of unused medications.
But there are still challenges for pill collections — most notably Nevada’s inability to get rid of them within state lines. Nevada Attorney General Adam Laxalt noted that the pills law enforcement gathers must be trucked to Utah or California because Nevada doesn’t have its own incinerators.
It’s also hard to accept syringes that could poke and infect the person collecting them, and groups collecting the pills must find secure locations to store them so they’re not stolen.
Laxalt has proposed buying five new drug incinerators with funds Nevada was awarded in a settlement with Volkswagen. The furnaces would go in Boulder City, Elko, Las Vegas and Reno or Lockwood and are pending approval from legislators on the Interim Finance Committee.
A sixth incinerator in Carson City, which has stood dormant because of environmental hurdles, is also coming online, Monroy said.
6. ROOTING OUT DRUG CRIME

Law enforcement agencies at the state, local and federal levels are working together to track down people who traffic illegal prescription drugs and run “pill mills.”
Attorney General Jeff Sessions announced on Aug. 2 that he was launching an opioid fraud and detection unit that will station experienced assistant U.S. attorneys in 12 states, including Nevada, for a three-year term. The lead prosecutor in Nevada is Kilby McFadden, who said she would spend her time targeting high-volume criminals and bad actor pharmacies.
She collaborates with the FBI, which has congressionally funded special agents who are based in Reno and Las Vegas and have recently launched four new investigations. Already, the FBI played a key role in the Reno pill mill case that was linked to Yenick’s death.
The FBI is part of a health-care fraud task force that, pending legislative approval, will also include a new investigator funded by the Nevada attorney general’s office. Having a state employee on the task force will make it much easier for the group to access data on the heavily secured Prescription Monitoring Program database, FBI agent Christina Burt testified at the task force meeting.
The Drug Enforcement Agency, which says Nevada is a source state for drugs that end up elsewhere, is also involved. The agency said it has sponsored 122 hours of free training to law enforcement about opioids and diversion and has distributed overdose kits to the public.
At the state level, the Department of Public Safety helps licensing boards look into possible prescription fraud cases. Since 2015, it has received 94 referrals from the pharmacy board, about half of which have evolved into full-fledged investigations. It's also initiated about 100 more probes based on other tips, according to Investigation Division Chief Patrick Conmay.
7. SUBPOENAING PHARMACEUTICAL COMPANIES

As the state continues the fight against opioid abuse on the ground level, a broad group of top prosecutors is trying to hit the issue at the source — drug companies.
Laxalt announced earlier this month that he’d joined a bipartisan coalition of 40 attorneys general to address the opioid crisis in Nevada and elsewhere. The prosecutors have served subpoenas on manufacturers of prescription opioids including Endo, Janssen, Teva/Cephalon, Allergan and Purdue Pharma.
They’re also demanding information from opioid distributors including AmerisourceBergen, Cardinal Health, and McKesson.
Laxalt says the information will help the coalition determine whether the pharmaceutical companies were breaking the law in their marketing, sale and distribution of opioids.
Support Local Journalism
Your contribution helps us provide free, independent news for our community. Join us in keeping local journalism alive.
Choose an amount or learn more about membership
