As lawmakers again debate medical aid in dying, patients and doctors say it’s far from simple

The California state border is less than 30 miles from Lynda Brooks-Bracey’s home.
A 57-year-old Las Vegas resident diagnosed with pancreatic cancer, Brooks-Bracey receives much of her treatment in the neighboring state, which has more specialty care options than Nevada. Her doctors say the cancer is metastatic, so widespread that it’s incurable.
Though she has access to treatment, therapies and medicine available to other cancer patients in California, as a Nevada resident, there’s one option she doesn’t have.
Medical aid in dying.
“It’s a state line. It’s a little border of earth to me,” Brookes-Bracey said in an interview. “I cross that border, and all of a sudden, my choices are different.”
California legalized medical aid in dying in 2016, allowing a physician to prescribe a lethal dose of medication for a terminally ill patient. It’s a practice authorized in 10 states and Washington, D.C.
As Nevada lawmakers again consider legalizing medical aid in dying, Brooks-Bracey hopes the Legislature approves it as an option for patients like her.
“Even if [the bill] is passed tomorrow, it probably won’t help me,” she said. “But I pray and hope that it will help somebody down the road.”
A Christian and self-described believer in God with four adult children, Brooks-Bracey is on palliative chemotherapy treatment, a type of care to ease symptoms and give a patient more time even if there is no cure for an illness. She’s hoping chemotherapy can give her the time for a clinical trial to become available to help extend her life.
But when hospice care can give no relief from pain, and she’s no longer herself, Brooks-Bracey said she would like access to the option to pass away on her own terms.
“[Hospice care providers] do a phenomenal job. But … they cannot do everything,” she said. “They cannot guarantee a lack of suffering.”


‘Soul searching’
2023 marks the fifth legislative session where Nevada lawmakers have debated a measure to legalize life-ending medication for terminally ill patients. The issue is far from partisan and recent polling conducted by Susquehanna Polling & Research and sponsored by a pro-medical aid-in-dying organization indicates 82 percent of Nevada voters support legalizing the option.
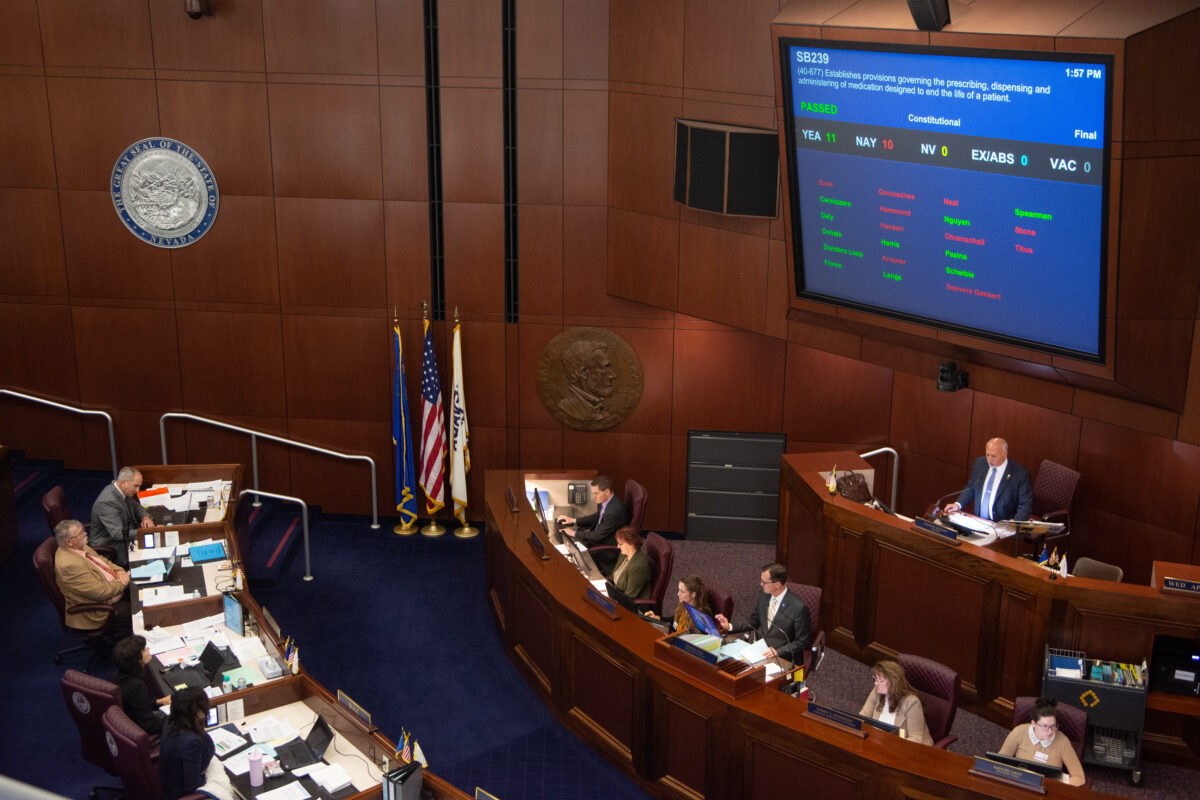
The furthest a medical-aid-in-dying proposal advanced prior to the 2023 session was in 2017 when a bill sponsored by then-Sen. David Parks (D-Las Vegas) passed through the Senate on an 11-10 vote with two Democrats and all but one Republican opposed.
Sen. Pete Goicoechea (R-Eureka) and Sen. Patricia Farley (I-Las Vegas) crossed party lines to pass the measure. In his floor remarks before the vote, Goicoechea said death is something everyone in his world deals with constantly: whether with an old dog, a good horse or a terminal animal.
He referenced the novel Old Yeller, saying sometimes those choices are hard and said that over the years, a number of his constituents who were close friends ended their lives after receiving a terminal diagnosis.
“For the families who are impacted by that, this bill and death with dignity would, in some cases, give them an option beyond using a hose to the exhaust pipe or a gunshot,” Goicoechea said. “Death with dignity is a far better option.”
Though then-Sen. Ben Kieckhefer (R-Reno) had been a co-sponsor of similar legislation in the past, he cast a vote against it, saying he felt a “lack of clarity” around the bill, which brought up questions for him about humanity’s divine spark and how people respect it.
Despite the 2017 bill failing in the Assembly, those sentiments were echoed in later sessions.
“It has made me do some soul searching and actually maybe do some research in the Bible because this is a very tough conversation for us to be having,” Assemblyman Gregory Hafen (R-Pahrump) said during a 2021 hearing on the measure.



That failed 2021 measure and the 2023 measure were sponsored by now-Sen. Edgar Flores (D-Las Vegas), who noted that he would have never expected to bring forward legislation legalizing end-of-life medication after growing up in a traditional Latino and Catholic household.
But after watching a family member suffer and pass away from a terminal illness, Flores said he wanted to give people facing a terminal diagnosis a choice about how to die.
“When you have a terminal illness, and you are suffering every single second, you’re not choosing between life and death,” Flores said during the 2023 bill’s (SB239) first hearing in March. “You’re simply choosing how it is that you want to die.”
The bill passed out of the Senate in a narrow 11-10 vote Wednesday, and now awaits a hearing in the second house.
A spokesperson for Gov. Joe Lombardo said the governor is aware of the legislation but did not comment on whether he supports it.
Legalizing medical aid in dying
Under Nevada law, terminally ill patients can refuse resuscitation or treatment to keep them alive, but they are prohibited from actively taking drugs to end their lives.
Medical professionals can also administer palliative sedation to terminally ill patients as a last-resort measure. Palliative sedation uses pain relievers and sedatives to alleviate suffering by making a patient calm, unaware or unconscious until they die from their illness. The process can occur in a hospital or home while a patient is in hospice. If palliative sedation takes place in an at-home setting while a patient is in hospice, families or loved ones often carefully manage the medication administration.
As proposed and amended, Nevada’s medical-aid-in-dying legislation has safeguards stipulating a physician can only prescribe life-ending medication to a patient who:
- Is at least 18 years of age
- Has been confirmed to have a terminal condition by at least two practitioners
- Has less than six months to live
- Has made an informed and voluntary decision to end life
- Has the mental capacity to make informed decisions (as determined by the provider or licensed mental health care professional)
- Has the ability to self-ingest the medication
- Is not requesting the medication because of coercion, deception or undue influence
The measure requires that patients requesting medication designed to end life must make two verbal requests, separated by a minimum 15-day waiting period. It also requires one written request signed by a witness who is unrelated to the patient, not entitled to any portion of the patient’s estate, not an interpreter for the patient and not someone connected to a health care facility.
Once a patient submits the requests, a practitioner must take the following steps:
- Inform the patient of the ability to revoke a request for medication at any time
- Determine and verify the patient meets all requirements for making the request
- Discuss diagnosis and prognosis as well as alternative options for care
- Refer the patient to a consulting medical practitioner who can confirm the diagnosis, prognosis and competence of the patient and that the patient has not been coerced or unduly influenced (the patient must then return to their primary doctor for the prescription)
- Instruct the patient not to self-administer the medication in public
The bill protects health providers from civil and criminal liabilities and states that they do not violate medical standards of care by assisting a patient in acquiring medication designed to end their life.
It also clarifies that wills, contracts, insurance and other annuity policies are unaffected by a patient’s decision to take life-ending medication. It also provides that no physicians or pharmacists are required to prescribe or fill a prescription for life-ending medication.
A death resulting from the self-administration of a medication designed to end a patient’s life would not constitute suicide or homicide. Patients would have their terminal condition listed as the cause of death on their death certificate.
‘Playing God’
Though supporters have described the end-of-life option as “medical aid in dying,” “death with dignity” and “physician aid in dying,” Dr. T. Brian Callister, a professor of medicine at UNR’s medical school and an internal medicine specialist and hospitalist, said those framings aren’t accurate.

“I call it physician-assisted suicide, or doctor-assisted suicide,” Callister said. “Words are important. And I believe [terms like ‘medical aid in dying’ is] candy coating physician-assisted killing.”
An outspoken and long-time opponent of medical aid in dying, Callister has been in the medical industry for more than 35 years and is considered an expert in hospital care transitions and end-of-life care. He’s traveled around the country testifying against medical-aid-in-dying legalization efforts and has focused on the need for better palliative end-of-life care and resources.
Callister, who is a parish deacon at the Lady of the Snows Catholic Church in Reno, also serves on a technical hospital patient harm panel through the Centers for Medicare and Medicaid Services and as the governor of Nevada for the American College of Physicians. He is the past president of the Nevada State Medical Association and the American College of Physicians Northern Nevada District. He said when he teaches about end-of-life care, he emphasizes the importance of keeping patients comfortable.
No doctor can accurately say when someone will die, he said. He added that doctors should do whatever they can to ensure a patient is comfortable and ease the pain of a terminal illness, but not end a life.
“Physicians shouldn’t be playing God,” Callister said. “I can give you a diagnosis. I don’t know how long you’re going to last. I’m going to say, who knows? Your Creator knows or nobody knows, however you want to believe it.”
He also said when people discuss end-of-life care, they often reference horrifying experiences with death, which he said can be avoided by pain management and proper end-of-life care.
“I’ve seen more selfless loving, more healing of family relationships, more bonding and closeness of families and friends during a terminal illness than you see at any other stage of life,” Callister said. “So as hard as it is, there are some incredible periods of growth and love, and relationships. And I think you risk losing a lot of that.”
Many supporters of medical aid in dying disagree. Numerous testifiers during the bill hearing in March spoke to the horror of watching friends and loved ones struggle with cancer before dying.
Reno resident R.J. Erickson told lawmakers how his father died after being diagnosed with stage 4 lung cancer. His father, John Marshall Erickson, had advocated for medical aid in dying and wanted to die peacefully. He said his father received hospice care but experienced a “torturous” death.
“During this end-of-life journey I was personally responsible for mixing his methadone and morphine. I was slowly killing my father,” Erickson said. “Over the five-day period, before he finally went into a medical or medicine-induced coma, there were episodes of hysteria, delusions … it was not what I was expecting to have happen.”

Many who testify to the horrors of watching family members die from a terminal illness have had terrible experiences with death, Callister acknowledged, but said modern medical care should ensure that kind of situation should never happen. He said those patients probably needed better palliative or hospice care.
Along with inaccurate predictions surrounding life expectancy and the commitment doctors make to cause no harm, Callister said he worries the legislation will have the unintended consequence of reducing access to care, because insurance companies will always go for the cheapest option and could deny payments for potentially life-saving treatments.
The legislation will likely make it so insurance companies will offer this so-called medical treatment of death in lieu of life-saving treatments that the patient may prefer, Callister said. He added that insurance companies denied care and instead offered the end-of-life option when he sent one patient to California and one to Oregon.
Others have raised concerns that the legislation could potentially harm communities of color that experience systemic inequalities in the health care system and issues the measure could present to people with disabilities who have historically faced barriers to self-determination and bodily autonomy.
Disabilities advocate Deidre Hammon wrote in opposition testimony that the legislation presents a form of ableism (discrimination and prejudice against people with disabilities) stemming from a fear of becoming disabled and thus a burden on family members. She added that “talk of legalizing assisted suicide for terminally ill patients could be expanded to include people who simply have lifelong disabilities.”
Proponents of the legislation argue that those types of concerns are addressed through the competency clause within the legislation and the requirement that patients make the request without any coercion and go through multiple hoops before receiving a prescription for life-ending medication.
Though students ask him what the correct dose of a type of pain drug is, Callister said the right amount is the one that works. Humans are adaptive creatures, he said, adding that pain medicines can be increased, there are regional nerve blockers doctors can employ, and there is no need for out-of-control pain.
As for the difference between a death via medical aid in dying and an overdose of pain meds, Callister said it comes down to intent. Suppose he or another medical professional gives a patient 10 milligrams of morphine and they die three hours earlier than they otherwise would have. In that case, Callister said that’s ethically different from medical aid in dying.
“We don’t know how much quality time we’re gonna have,” Callister said. “Let’s try to maximize that. And when you get near the end, I will do everything under my power to keep you comfortable and help you have a peaceful passing.”
Grappling with morality
Rabbi Benjamin Zober, one of the rabbis of Temple Sinai in Reno, said any conversation about death is often intertwined and heavily influenced by a person’s religious background and beliefs.
“Our society is death averse,” Zober said. “Religions often … end up taking a really hard line, whether we are active in a religion or not.”

He said Judaism places a high premium on personhood and the self, noting that within the religion there is a core belief that all humans are created in a divine image with a sacred spark. While studying to be a rabbi, Zober said he went through a battery of mock interviews and question sessions where he was asked about morals, ethics and practices, solidifying his beliefs and teachings.
But once he began working within communities, he said reality challenged his beliefs. For example, in Judaism, Zober said there are a set of rituals surrounding dying that he views as wonderful, but some families or individuals decline because that’s not what they want.
“It doesn’t pay to force someone into that mold because some book says so. The reality is that the person in front of us is different,” he said. “Sometimes that means that we have to rethink things.”
Other religious groups and organizations are explicitly opposed to medical aid in dying.
A statement from the Nevada Catholic Conference, a Catholic advocacy group, framed medical aid in dying as assisted suicide and said that the issue should not be confused with ethical end-of-life choices such as palliative care or hospice care.
“The Church believes in the dignity of all human life, until the moment of natural death. This vision is predicated on the conviction that God alone is the Author of life, and the sole arbiter of death,” the statement said.
A 2013 Pew Research report found that most major religious groups are generally opposed to medical aid in dying.
Zober said some interpretations of religious texts he’s read indicate that if there is something like pain stemming from a terminal illness that diminishes a patient’s ability to live in the image of God or severely threatens someone’s divine spark, then something like medical aid in dying would not only “be permitted, but it would be praiseworthy.” However, he said there have to be safeguards preventing abuse and careful consideration surrounding the matter.
“The problems with taking such a hard line about an issue, particularly one’s end of life, is that it can be very alienating,” he said. “If someone makes a decision and the people around them or the values of the people around them say, ‘this is absolutely not acceptable’ then there is no discussion … and possibly even no forgiveness. It puts that person in kind of an impossible situation.”
‘He begged us to help him die’
Based in the Lake Tahoe area, Dr. Johanna Koch is a board-certified family, hospice and palliative care physician who has practiced in Nevada for more than 35 years and as a hospice medical director for 20 years in the Silver State and neighboring California.
As a hospice physician, she has cared for approximately 3,000 patients with her teams and makes regular visits to check in on patients and assess their health. Though she works in both states, she said her patients face completely different options when it comes to end-of-life care.
Hospice can only do so much to mitigate pain and suffering, she said. At some point, patients feel as though the price of staying alive is too much — they face exhaustion, weariness, pain, nausea, weakness and other symptoms that are difficult to ameliorate.
“Sure, we can give you a pill that'll take their pain level down or manage their nausea, but that doesn't solve the bigger problem,” she said.

Though health care professionals will talk about how peaceful a hospice death can be, Koch said the reality is that waiting to die can be painful for patients and their loved ones.
She believes people who have unmitigated suffering and are at the end of their lives should have the right to choose how they die, whether that is through palliative sedation or medical aid in dying. Palliative sedation is often cast as a “natural death,” Koch said, noting that she doesn’t necessarily agree with that framing.
She said that if you are medicating somebody according to the law, all you're doing is sedating them enough that they don't wake up until they die. If a patient is well-hydrated and has a good fat mass on their body when that starts, they could live weeks. Their skin may start falling off and their body will start decomposing before their heart and lungs give out, she said.
“I'm not sure who judges the value of a natural death versus being empowered to have control over your own death,” Koch said.
Koch said she doesn’t discuss the option of medically assisted death with her patients unless they bring it up. She estimated she has prescribed the medication to fewer than 30 patients and said she has never moved forward on a patient’s request for aid in dying who she felt was being coerced or acting impulsively.
“I have to feel really good and clean about every prescription I write,” she said. “[People requesting medical aid in dying] have done soul searching, they've done everything they needed to do to bring closure in their lives. … they've made amends, they're ready to go and it's just so clear.”
When working with patients in California requesting medical aid in dying, she said she’ll probe their intent, asking questions about whether they know what they’re asking for, why they might want to end their own lives and the consequences of that decision.
Not having that option available in Nevada can lead to more agony for patients, Koch said.
“It also makes me worried that they may take things into their own hands,” she said.

In all her years of practice, Koch has only had two patients commit suicide. She and her hospice team take precautions to prevent overdoses, including closely tracking medication use and ensuring there are mental health resources available to patients.
Most of her patients in Nevada are unaware of the option of medical aid in dying because it’s not legal in the state. But two years ago, Koch said she had a patient at Summit View Hospice in Reno with advanced cancer that no longer responded to treatment.
He was suffering and the drugs needed to control his pain rendered him too sedated to function. She said he frequently expressed a desire to die.
“We provided spiritual, emotional and psychological support, frequent visits and aggressive symptom management,” Koch said. “Despite this, he begged us to help him die.”
She described how on a cold winter morning, her patient called the police and informed them there was a dead body in the garage. He then went into his garage, spread out a tarp, laid down and shot himself in the head.
“That broke my heart,” she said.
Finding comfort
For some, the option to die on their own terms brings its own comfort.
In the past, Koch said she has prescribed end-of-life medication to a patient who was then willing to try a more aggressive form of chemotherapy because she knew she could opt out if the suffering became too much. The patient eventually did not take the medication.
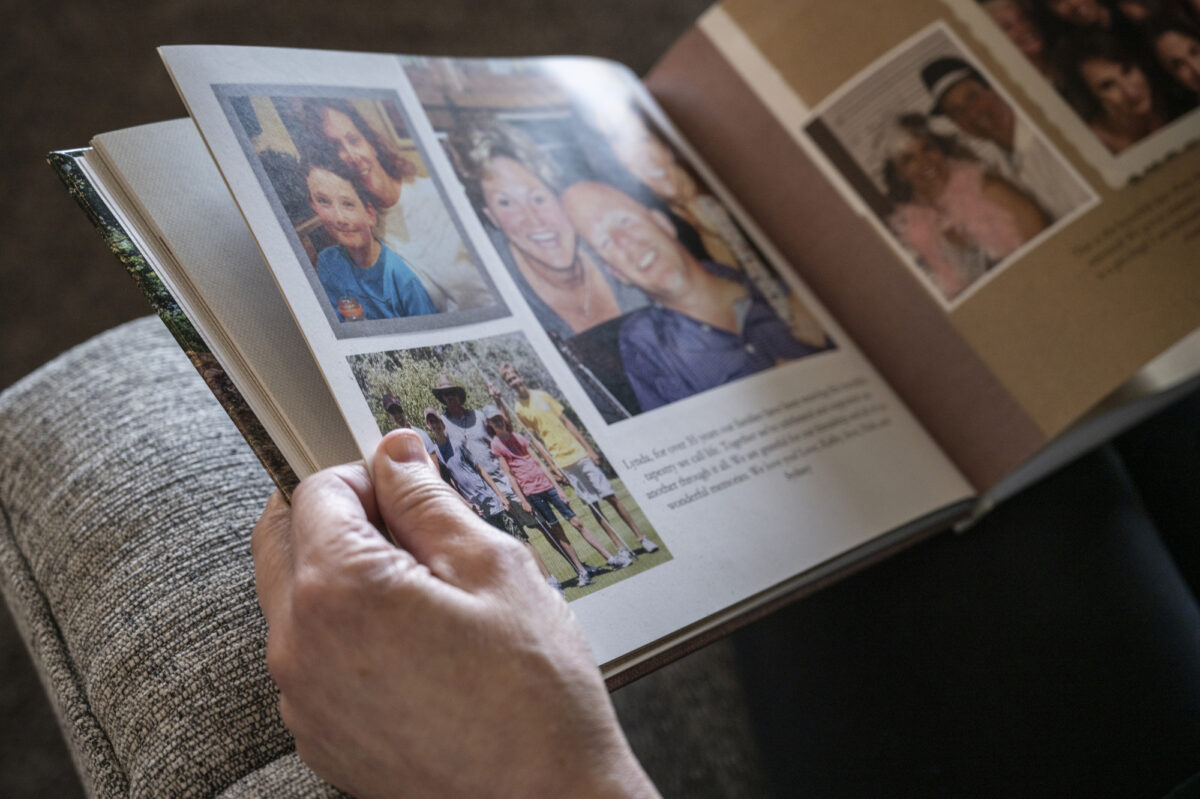

For Brooks-Bracey, this isn’t her first time facing death.
More than 20 years ago, her first husband died after he was diagnosed with leukemia. Brooks-Bracey said he received wonderful hospice care, but he still died in pain.
People don’t talk about death and dying, and how it happens, she said.
“Most people do not pass away as we assume or hope that they do in the movies and in the fantasies that we see,” Brooks-Bracey said. “It doesn’t always happen that way. Even with the best intentions from doctors and hospice, they can still only do so much.”
