IndyFest: Insured rates up, but Nevada Medicaid still struggles decade after expansion
Nearly a decade after Nevada implemented Medicaid expansion under the Affordable Care Act, the results are in — the state's uninsured rate has plummeted, but challenges still plague the state's health care ecosystem.
Through the pandemic, Nevada Medicaid saw a historic rise in enrollment, leading to about one in three Nevadans being covered under the health insurance program for low-income people and those with disabilities. But as the state resumes eligibility checks post-pandemic, reporting indicates that Medicaid coverage has been canceled for more than 169,000 Nevadans.
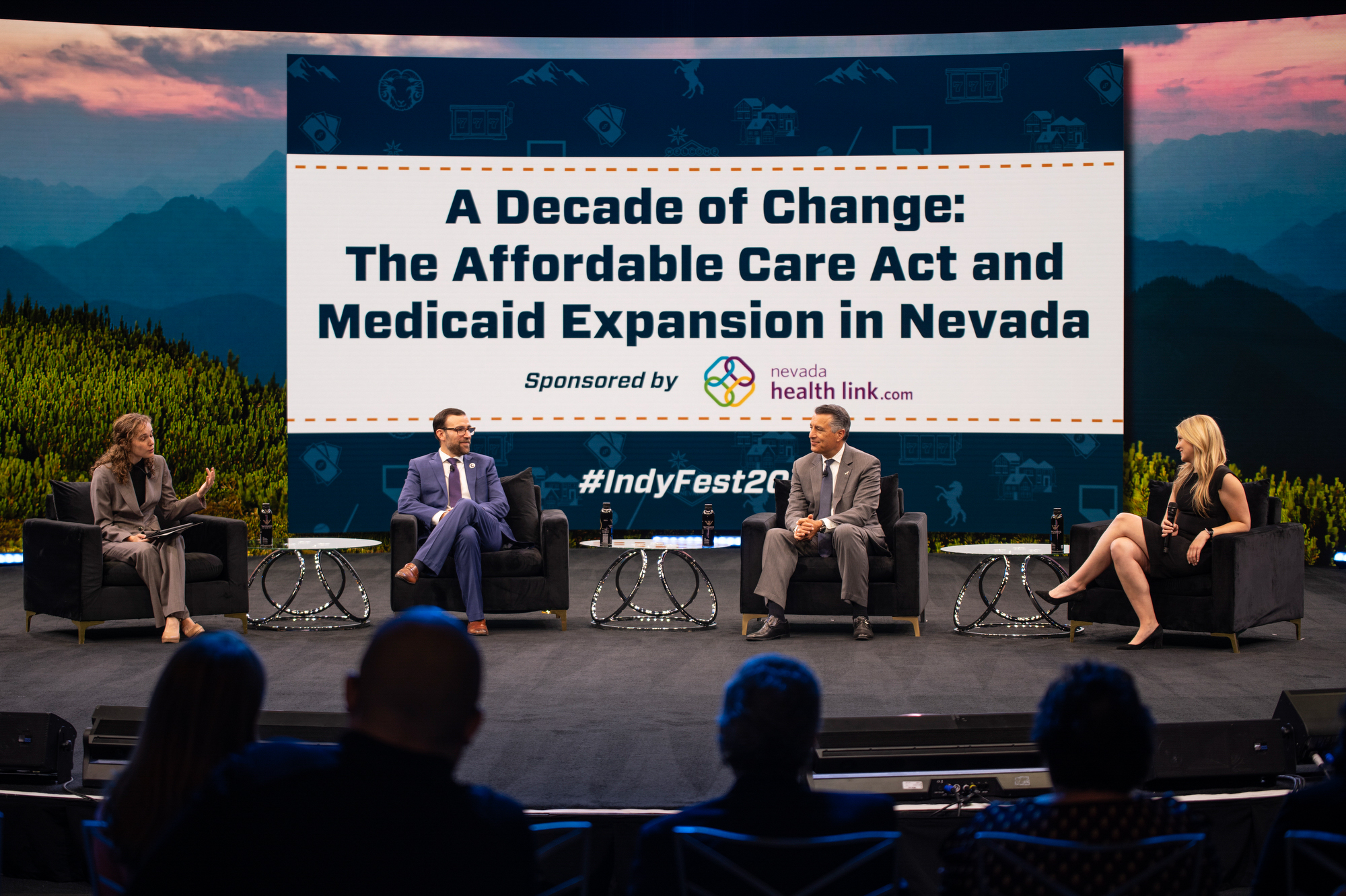
During a 50-minute panel discussion at The Nevada Independent's annual politics and policy-focused IndyFest conference, UNR Associate Professor Dr. Jose Cucalon Calderon, Politico reporter Megan Messerly and UNR president and former Gov. Brian Sandoval discussed Medicaid expansion since its implementation in 2014, including changes following the end of the pandemic-era "continuous enrollment" policy.
Messerly, who has tracked how the unwinding has affected states across the country, said the continuity of coverage policy adopted during the pandemic allowed states to ensure people were covered during an unprecedented health crisis. But it was expensive, and states are working through the unwinding process at different speeds.
"You can see the raw totals of how many people in Nevada and elsewhere have lost coverage. The question is, are those folks going to employer-sponsored coverage?" Messerly asked. "Or are those folks going uninsured?"
Though the unwinding is a return to pre-pandemic policy, Cucalon Calderon said the re-enrollment process has hindered qualified patients' ability to remain on Medicaid.
"I have had a lot [of] patients cancel their appointments," Cucalon Calderon said. "Either they filed it incorrectly, they didn't understand what the paper was, or they just had to deal with three jobs and five kids and not being able to put things on time."
The three panelists also spoke about a host of other topics, including cultural barriers to health care, political responses to Medicaid expansion and more.
To watch the full panel, click here. We've highlighted parts of the discussion below.
Politically tenuous decision
In 2013, Nevada's uninsurance rate was at 23 percent — the highest in the country. Sandoval, who was the first Republican governor to commit to expanding Medicaid under the Affordable Care Act, said that at the time, the state did not offer Medicaid coverage to single, childless adults, and the threshold for children was high.
He said the state was also facing a mental health crisis, and hospitals were filled with patients who needed mental health services and couldn't get them elsewhere. Though there was political pressure not to accept Medicaid expansion, Sandoval said it made sense.
"At that time, we went from 200,000 to 600,000 people that had coverage, and now it's over 900,000," Sandoval said. "So there are a lot of individuals in the state that have coverage that would not otherwise have it."
In 2017, Sandoval was a fierce defender of Medicaid expansion at a time when Congress was trying to repeal and replace the Affordable Care Act.
Sandoval said that politically, the decision was difficult, but it wasn't a hard choice to make.
"I knew what it had done for our state, and the results spoke for themselves," he said. "I got a call from the president himself encouraging me to talk to Senator [Dean] Heller … he was a gentleman about it, but I said I have a fiduciary duty to the people of my state, and this is in the best interest of the people of Nevada."

Uninsured rates and preventative health care
Analyses of 2021 data by the United Health Foundation indicate that Nevada's uninsured rate has dropped to 11.6 percent. Reporting from the nonpartisan Guinn Center notes that the majority of uninsured people consist of young adults, Latinos, less educated people and lower-income individuals.
Cucalon Calderon said that many of his patients struggle with knowing where to go for care and distrust the medical community. He estimated that about 90 percent of the parents of his patients are not accessing preventative care.
"Part of the barrier is not knowing, the other barrier is the fact that in Latin American cultures, preventive care is just something that just is not the way that the health care system is structured," he said.

Weathering the pandemic
Messerly said that at a basic level, having more people on Medicaid during the pandemic allowed them to get preventative care and see a doctor more regularly, limiting visits to the emergency room or other high-level care needs.
The expansion also helped increase vaccination rates and encouraged people to take care of themselves.
However, Sandoval noted one difficulty with Medicaid expansion is a lack of physicians taking Medicaid patients, and that's partly because of low reimbursement rates.
"One of the challenges now is to increase those reimbursements so that more physicians are willing to take Medicaid patients," Sandoval said.
Cucalon Calderon added that for about five years, he was the only Medicaid-exclusive pediatrician who spoke Spanish as a native speaker. During that time, he said he had to refer patients out of state to get care or to other areas of the state.
"They ask us for alternatives all the time, because the care that they are receiving is just too difficult to be able to access," he said.
As Nevada and other states take on the challenges of Medicaid re-enrollment, he said it is essential to invest in infrastructure and resources to ensure that people can receive help if they continue to qualify for Medicaid. And if patients don't qualify, Cucalon Calderon said there should be an emphasis on finding ways to help them continue securing care.
Messerly said dis-enrollments for administrative reasons, such as lost documentation or inability to reach patients, are taking place across the county.
"There are people who are falling through the cracks," Messerly said. "How do we move through this process efficiently to remove the people who are actually ineligible, but not move so fast that we lose so many of those other people who are losing coverage sort of for accidental reasons?"

Solutions to a provider shortage
Sandoval said one of the solutions to the state's provider shortage is expanding and better funding graduate medical education with a goal of increasing residencies in the state.
"Residents will stay 70 percent of the time where they've done the residency," he said.
Sandoval said the more money the state invests in Medicaid, the more money they get back from the federal government, which could also help increase the reimbursements for Medicaid providers.
Messerly said another option is the Basic Health Program offered through the Affordable Care Act, which covers those under a certain threshold of the federal poverty level whom Medicaid does not capture.
Issues with personnel and antiquated technology are also to blame for the provider shortage and delays in reimbursements for doctors, panelists said.
"When we think about the technological challenges of Medicaid, there's so many, and it's because so many of these systems are so old, and even changes we would think might be really simple are extremely complicated," Messerly said.
On the provider side, Cucalon Calderon said it can be difficult to know what treatments are covered for patients if their insurance situation is in flux.
"It's really difficult to keep up," he said. "It's a really large time-consuming thing because this delays patient care as well. And our patients don't get their prescribed treatment on time either."
Support Local Journalism
You’ve enjoyed unlimited access to our reporting because we’re committed to providing independent, accessible journalism for all Nevadans.
But sustaining this work — informing communities, holding leaders accountable, and strengthening civic life — depends on readers like you.
Nevada needs strong, independent journalism. Will you join us?
A gift of any amount helps keep our reporting free and accessible to everyone across our state.
Choose an amount or learn more about membership
