As Nevada grapples with high suicide rates, Elko mom finds tragedy ‘does not discriminate’

Content notice: This article discusses suicide, suicidal ideation and suicide attempts. If you or a loved one are struggling, it’s OK to share your feelings, and there is free and confidential 24-hour support available in Spanish and English at the 988 suicide and crisis phone line. For mental and behavioral health services in Nevada, click here.
This is the first in our multipart ‘We’ve got to talk’ series, which focuses on youth mental health in Nevada and is produced as part of the USC Annenberg Center for Health Journalism’s 2024 National Fellowship Kristy Hammam Fund for Health Journalism.
Kade Lesbo was a left-handed pitcher with good control and a strong makeup.
His junior varsity baseball coach described him as a mentally tough kid with a positive, uplifting attitude, who never seemed to get rattled.
He loved the Seattle Mariners, riding dirt bikes, hunting, fishing and camping.
Friends and family described him as someone who didn’t seek attention but was well-liked and quick-witted, with a comeback to anything. He had a steady girlfriend and enjoyed spending time with his cat, Addie, and golden retriever, Liv.
Kade even helped his parents build their dream house in Elko and hoped to someday take over his dad’s custom welding business, Battleborn Fabrication, after graduating from college.
But on Sept. 12, 2022, the high school junior walked into his parents’ room while his mom was cooking pork chops in the kitchen. There was a gun in the closet, and Kade used it to shoot himself in the head.
Initially, his mom, Louri, said his older brother thought he had fallen on one of the shelves and cracked his head open. But Kade, 16, had found the hidden ammo.
Data from the Department of Health and Human Services’ Office of Analytics shows that Kade was one of 77 people between the ages of 15 and 24 who died by suicide in the state in 2022. Since 2010 — the earliest state records date back to — it’s an age group that has the highest rate of suicide attempts of any other age group in the state. But other age groups have consistently represented a higher proportion of deaths from suicide, with those older than 85 making up the highest rate.

A first-grade teacher, Louri, said she never would have thought her son would die by suicide. It isn’t supposed to happen in a supportive, caring family.
“We are those parents that just love our kids beyond belief,” she said. “We were immune to suicide until we were not.”
Elevated rates in Nevada
Kade was born and died in northeastern Nevada’s Elko County, the state’s second-largest county covering more than 17,000 square miles, with a population of about 54,000 people. Mining, ranching and gaming dominate its economy.
In 2020 a state report shows Elko County had the highest youth and young adult suicide death rate of any of Nevada’s 17 counties, with 40.6 deaths per 100,000 county residents between the ages of 10 and 24.
State officials declined to say what county had the highest rate as of its most recent data but did note it is no longer Elko County.


The state does not publicly report the number of suicide deaths in each rural county because it would violate Nevada’s data suppression rule, which aims to maintain confidentiality on aggregate data. So there’s no specific number of how many people died in Elko County the same year as Kade. Officials said rural regions’ low population counts mean that rural counties frequently report only a few deaths from suicide each year, leading to wide variation in those counties’ rate of deaths from suicide.
But the state health department’s office of analytics offers regional data. Clark County, Nevada’s most populous county, has the lowest rate of suicide deaths and, as of 2023, saw an 11 percent decrease in deaths from the previous year. The state’s second-most populous county, Washoe County, saw a 4.4 percent decrease. In contrast, rural counties in Northern Nevada (which includes Carson City, Douglas, Storey, Lyon and Churchill counties) saw a more than 36 percent increase. Rural counties in Southern Nevada (Mineral, Esmeralda, Nye and Lincoln counties) had a 26 percent increase and had the overall highest rate of deaths by suicide.
The final rural region, which includes Elko, White Pine, Eureka, Lander, Humboldt and Pershing counties, saw a more than 10 percent increase.
Reporting from the health care research and analysis organization KFF indicates that nationwide, suicides are most prevalent among those living in rural communities, men, Native Americans or Alaska Natives and white people, and are rising among communities of color, younger people and residents of rural areas.
Misty Vaughan Allen, Nevada’s suicide prevention coordinator, said Nevada’s suicide rates have held relatively steady since 2010, which she said is primarily because of more community tools, increasing partnerships to address mental health needs, rising awareness of mental health issues and less stigma surrounding seeking therapy.
She attributed decreases in suicide deaths in urban parts of Nevada to growing suicide prevention help through the state’s text or call options, partners doing suicide prevention work and a workforce with more effective skills to recognize and intervene when someone has suicidal thoughts. Vaughan Allen said isolation, lack of resources and rural communities’ boom and bust economies contribute to higher suicide rates in those areas.
And then there’s access to lethal means. In 2023, firearms accounted for more than 61 percent of suicide deaths in the state, higher than the national average of 55 percent (as of 2022). Firearms are also one of the most lethal means of suicide, often used within 10 minutes of suicidal thoughts.
A KFF analysis indicates that twice as many suicides by firearm take place in states with the fewest gun laws, relative to states with more laws.
“Nevada is a higher gun-owning state, and with that comes higher deaths of suicides by firearms,” Vaughan Allen said.

Creating change
Nevada is one of nine states within the U.S. considered to be part of a “suicide belt” where the suicide rate is much higher than the national average. Nevada has the 11th-highest suicide rate in the country, and suicide is the most common cause of death for Nevadans aged 12-19, and the second leading cause of death for residents aged 20-46.
On average, 12 Nevadans die by suicide each week, which is higher than combined deaths from motor vehicle crashes and homicides.
In the months after her son’s death, Louri wracked her brain for warning signs she may have missed. She thinks about the day he died. Kade had been fitted with an extremely tight retainer, which gave him a lisp and frustrated him. A month earlier, he’d had surgery after he tore the ligaments on the inside of his elbow while pitching and his recovery was expected to take a year or more. Right before his death, she said he seemed to experience a sense of euphoria, which can be a sign of an impending suicide.
But with no way to definitively know why Kade died by suicide or change the past, Louri said she wanted to find ways to help prevent suicide from affecting other families.
Kade was a well-known, well-liked athlete in a rural community centered around sports. A month after his death, another well-known high school athlete in the community died by suicide.
Louri, her family and the community rallied, pushing for a school district policy for what happens after the death of a student or staff member, helping establish a peer-to-peer mental health network known as the Hope Squad, and advocating alongside a local nonprofit to bring information about suicide prevention throughout the county. The changes also align with mandates requiring suicide prevention training be offered to students, teachers and administrators for middle and high schools — implementation that experts say has been slowed by the pandemic and resource availability.

Alongside the advocacy, the state and other partners have established a children’s mobile crisis team, funded community co-response efforts such as virtual crisis care visits, provided avenues for therapy, connected residents with medication safes, and used COVID-19 relief funding to implement mental health programs and services designed to outlive the temporary aid.
Vaughan Allen said the state also has a program offering free gun safes to families. She said having a safe can increase the barriers to using a gun to harm oneself, giving the person some time to think and professionals time to get that person help or time to self-de-escalate.
A measure passed during the 2023 legislative session required the Department of Health and Human Services to establish a safe firearm storage education campaign and for school districts to develop plans for schools responding to suicide.
Vaughan Allen said there’s a stigma surrounding discussions of suicide, but during the last two decades, that has slowly shifted. She said the state has seen increasing levels of funding and policymakers supporting mental health and suicide prevention, which makes it more likely that prevention activities last in the long term.
Vaughan Allen added that Elko has been working for years with Zero Suicides Elko County, the nonprofit dedicated to preventing and addressing suicides, so there was an element of readiness and support for families when their young people died.
“What I don’t like to see is we coalesce under tragedy, and then after a few months people don’t want to talk about it anymore because it’s heavy and scary,” Vaughan Allen said. “And then we’re right back where we started.”
Leading up to Kade’s death, Louri said his brother, Kason, who graduated high school in 2022, had a classmate die by suicide every year since 2018.
Following the advocacy and conversations, Louri said that no one at Kade or Kason’s high school has died by suicide since 2022 that she knows of.
Louri said she doesn’t know if the changes that have taken place since Kade’s death would have happened if it wasn’t for someone well-known in the community dying by suicide and her family’s and others' willingness to talk about what happened.
“Suicide does not discriminate. I’m here to attest to that,” she said. “We’ve got to talk about this. I wish somebody had brought that to my attention.”

Understanding the risks
Michelle Sandoval, a licensed clinical social worker and a clinical program manager at the Nevada Division of Public and Behavioral Health’s rural clinics, said mental health issues in rural counties stem in part from limited mental health options, isolation, transportation challenges and, in mining communities such as Elko, long shift work with irregular schedules.
Sandoval said children whose parents work odd hours are often left fixing dinners and doing homework alone, unable to get to events and with more responsibilities than their peers living in more urban settings.
There’s also a technological and cultural gap between parents and children, she said. The world is running so fast, Sandoval said, and there’s constant access to information and social media, which leads to a hypervigilant state, and, consequently, more anxiety and depression.
“We used to call it fight, flight or freeze, and you would go into it when you didn’t feel safe,” she said. “Our youth nowadays are constantly in that fight, flight or freeze arousal state.”


In interviews with The Nevada Independent, teenagers living in Elko County shared some of their thoughts about mental health in rural communities.
Sophia Wintermote-Bribiesca, a 13-year-old eighth grader, said it’s sometimes easier to talk to a stranger about mental health in a tight-knit community such as Elko.
“It's hard when you're going through a rough time to say anything, because everybody knows you, and you don't want to make your parents look bad,” she said. “My mom is a great mom, but sometimes it gets a little hard … and we still argue.”
Lillian Harney, 17, attends high school in Wells and is part of the school’s peer-to-peer mental health support group, the Hope Squad. As a member, she’s trained in how to talk to peers about mental health, catch suicide warning signs and know when to seek help from adults.
She said her parents work long hours, and as the eldest child, she takes on added responsibilities. Harney said having extra responsibilities can give kids anxiety because they don’t have anyone to talk to about their stress. The Hope Squad, she said, is a place to turn to for struggling youth.
“A lot of times Hope Squad is misinterpreted like it's just strictly about suicide, but in reality, it's more like seeing how others are, their mental health and noticing people so not everyone feels alone,” Harney said.
Deciding to stay
Unless a suicide takes place in a public place, law enforcement is not responsible for cleaning up afterward, though some homeowners insurance policies do cover the costs.
Louri said there were no cleanup services in the county when her son died, and two of their good friends and her father-in-law cleaned up the closet.
“They did that to shield us,” Louri said. “It was the nicest act of kindness.”
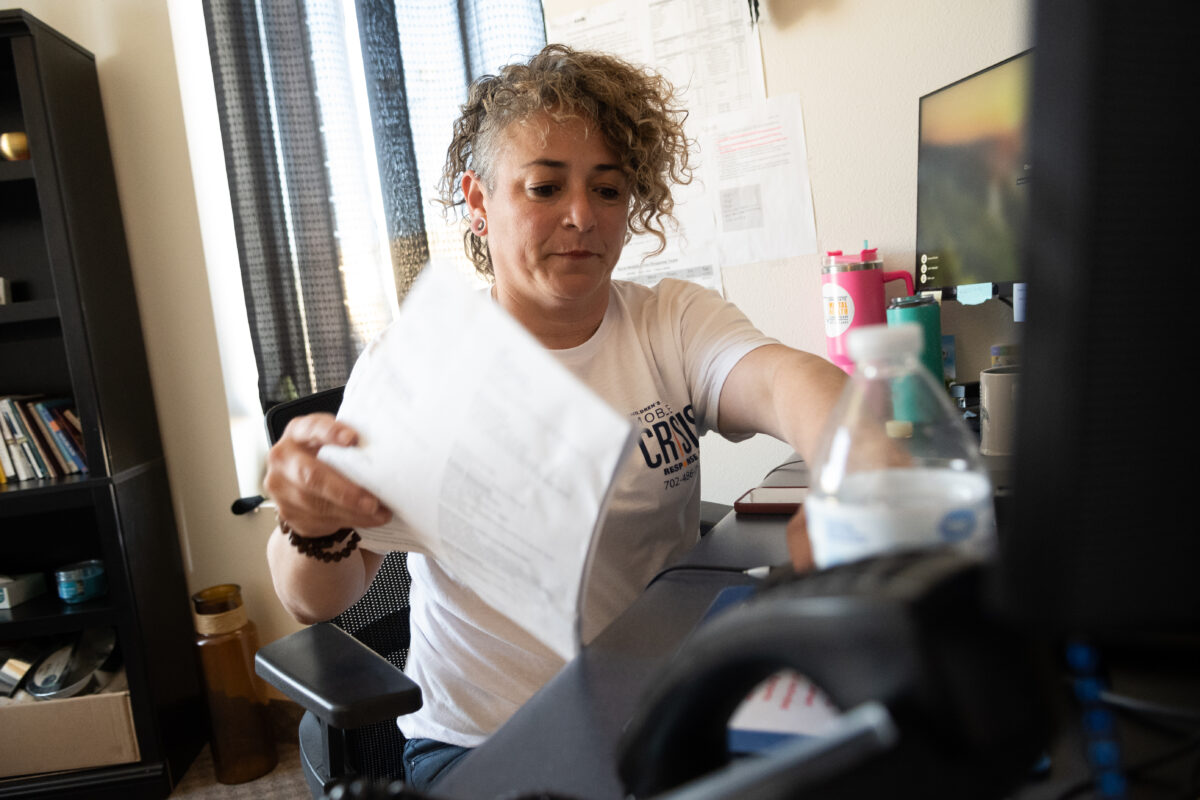
Since her son’s death, Louri joined Zero Suicides Elko County, which has offered her grief support and a way to work to prevent other suicides from happening. She said she is willing to talk about her son because conversations around mental health and suicide prevention need to take place.
But the pain and loss are still there. Following Kade’s death, the family’s cat, Addie, wandered through the house, searching for him.

After the blood stain was painted over and the carpet was replaced, Louri and her family wondered whether they should stay or leave the house they had built with Kade.
They left the decision up to their other son, Kason, who said he wanted to stay because it felt like a part of his brother was still there.
“We built this,” Louri said. “At first, you’re like, no way, I’m not going to stay here. I can’t. But then my counselor’s like, ‘You need to reframe your thinking. That was also the place that he left, but he put so much of his life into it, too.’”
