Meeting Nevadans’ mental health needs challenged by limited resources, isolated efforts

Content notice: This article discusses suicide, suicidal ideation and suicide attempts. If you or a loved one are struggling, it’s OK to share your feelings, and there is free and confidential 24-hour support available in Spanish and English at the 988 suicide and crisis phone line. For mental and behavioral health services in Nevada, click here.
This is the third in our multipart ‘We’ve got to talk’ series, which focuses on youth mental health in Nevada and is produced as part of the USC Annenberg Center for Health Journalism’s 2024 National Fellowship Kristy Hammam Fund for Health Journalism.
You can read the first story here and the second story here.
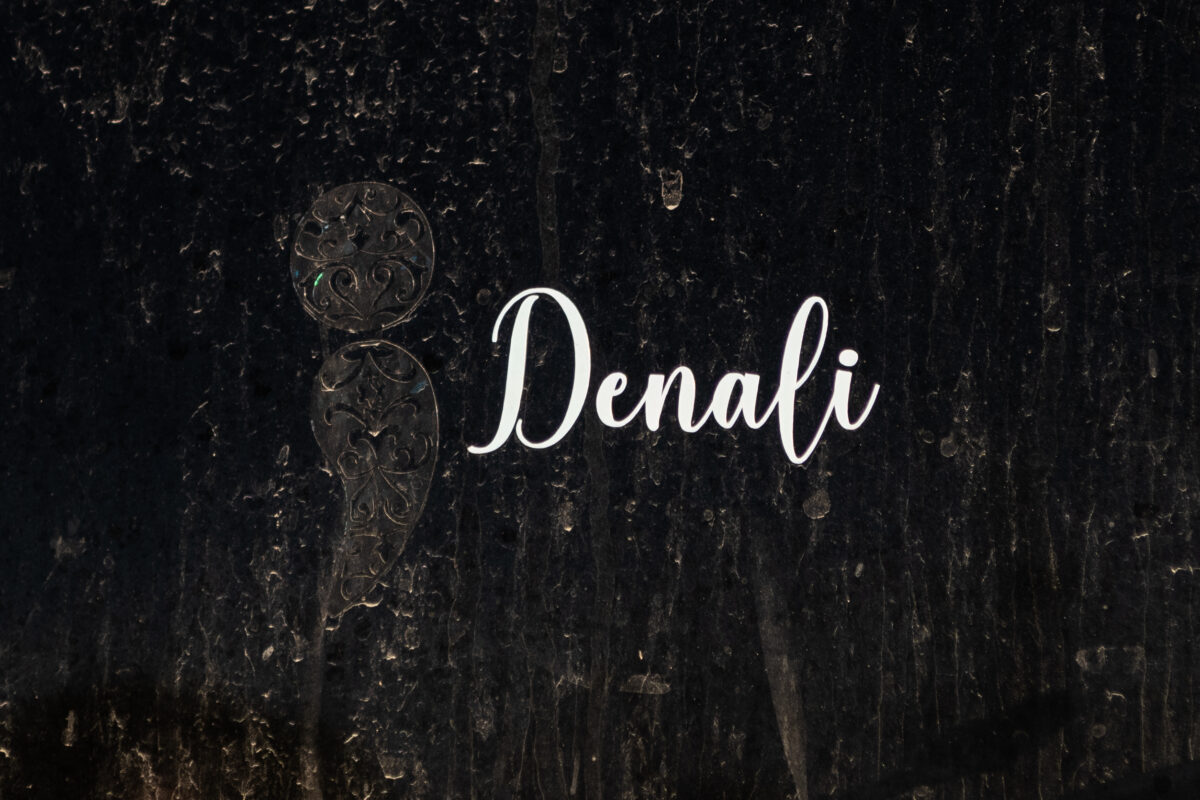
Four weeks after his son, Denali, 16, died by suicide in 2018, Jason Mayne went back to work.
Given a month to grieve, Jason thought he could return to his job as a health and safety trainer for Nevada Gold Mines in Elko County, as usual. But after he responded to a fatality at his workplace, the nightmares and panic attacks began and would not let up.
Jason realized he needed help processing his son’s suicide.
“It was blatantly obvious to everybody else. I couldn’t deny it,” he said.
He reached out to a doctor he met at work who drove more than four hours from Reno to provide him with support and guidance. But Jason and his wife, Denali’s stepmother, Sarah, found it difficult to seek long-term therapy options for their family and two young children, aged 9 and 11.
“Once the numbness had really worn off, it was time to find somebody that [the kids] could really work with, help them carry the grief better,” Sarah said. “So then we did start actively looking, and there just wasn’t anything here for them.”
Jason and Sarah eventually started making weekly five-hour round-trip drives to Twin Falls, Idaho, to have their young children receive play therapy.
More recently, he and his wife’s longtime counselor moved to a different practice and they have been trying for weeks to get the therapist reapproved by insurance.
“Other people’s lives go back to normal, and your life never will,” Jason said.
The family’s struggles to find children’s therapy are common in rural Nevada. Data from UNR’s 2023 Nevada Rural and Frontier Health report shows that in 2022, there were only 342 licensed psychologists in Nevada, including nine in rural and frontier counties.
Geography and scarcity aren’t the state’s only challenges. Nevada has a fragmented system of care options and a lack of sustainable funding that hinders the development of a more unified network of supportive services.
Natasha Mosby, a licensed clinical social worker with UNLV, has witnessed the need for coordinated services.
“[Pediatricians] may have a kid in the office, and their first step may be to say they need to go to the hospital,” Mosby said. “We have a team here that will support that doctor, the family, and to keep them in their homes, safely secured with those wraparound supports.”
Mosby oversees the Nevada Pediatric Access Line (NV PAL), a free child psychiatry access program designed to bridge service gaps and help children receive comprehensive care. The program is funded through a federal block grant managed by the state.
The state’s behavioral health system relies upon state general funding, federal grants and Medicaid, the government insurance program primarily serving low-income people. The various funding sources often have differing requirements and goals, which can lead to inflexibility, efforts that are not being coordinated by a single overarching entity and financial uncertainty if federal funding priorities change and grants end.
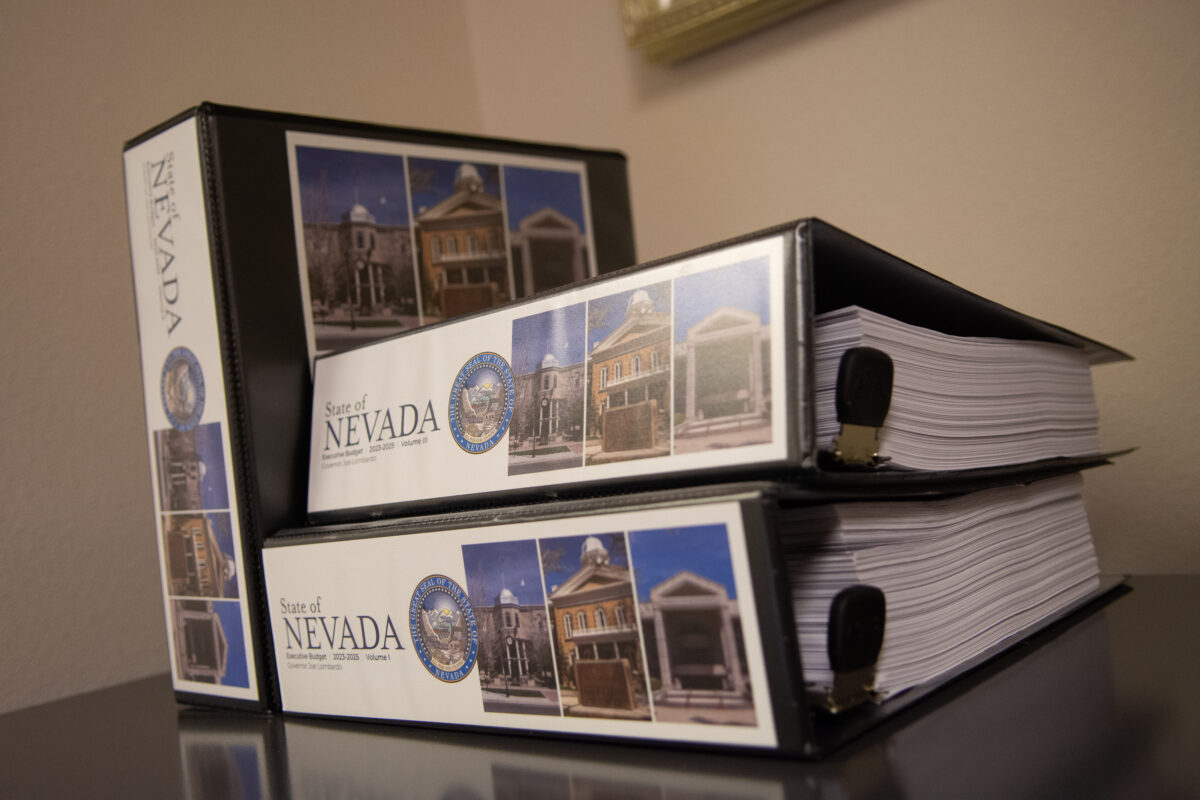
State records show that in fiscal year 2024, about $1.65 billion was spent on programs supporting behavioral health — the connection between behaviors and the well-being of the mind and body, which includes mental and physical health.
Some 40 percent of the funding came from state general funds, 52 percent from federal Medicaid funds, 7 percent from federal grants and American Rescue Plan (ARP) funds and the remaining 1 percent from other sources.
As federal lawmakers discuss how to make room in the budget to extend tax cuts that are expiring soon, Heather Saunders, a senior research manager at the independent health policy research organization KFF, said it appears that Social Security and Medicare are off the table. However, Medicaid hasn’t been mentioned. Saunders said states, including Nevada, could face difficult budget decisions if federal Medicaid spending is cut.
“It’s hard to know what exactly the federal government will do at this point and also how states will respond,” Saunders said. “In Nevada, Medicaid covers 3 in 8 children so that means there could be implications for mental health and substance use disorder coverage and access to care.”

Federal funding uncertainty
Nevada is ranked worst in the nation for its youth mental health services. With nowhere to go but up, the state has made progress to address it.
But those efforts could regress if federal funding sources dry up.
In 2024, Nevada finalized a contract to expand crisis response services through the 988 hotline, which was funded in part by an unprecedented allocation of money for mental health services from the American Rescue Plan. Mental health advocates, experts and state workers applauded the funding, which supported youth care, case management and established a children’s behavioral health authority and other vital projects.
Of the more than $514 million Nevada’s Department of Health and Human Services received through the American Rescue Plan, state records show about 22 percent supported behavioral health efforts for children and adults.
Underscoring the state’s support for mental health initiatives is the record-setting commitment of nearly $200 million during the next three years. The funding is derived from an expanded tax on hospitals implemented during the 2023 legislative session; officials said it aims to “transform” Nevada’s behavioral health care system for children in foster care and with significant behavioral needs.

Despite the new spending, most of the state’s progress hinged on federal COVID-19 aid.
Carissa Pearce, the Children’s Advocacy Alliance of Nevada health policy manager, said many state agencies have secured funding for at least the next year but are unsure what will happen in the following fiscal year.
“We’ve only been building [the mental health] workforce for a very short amount of time, and with the potential to lose out on a huge revenue source, we may be going backward,” she said.
Shannon Bennett, a bureau chief for the state’s division of public and behavioral health, said the COVID-19 funds were used for one-time projects or to set up programs with a long-term funding plan, such as ones reimbursable through Medicaid.
“The funds are really used to bolster and build things that hopefully then can go off and fly on their own,” Bennett said.
Bennett said federal block grants for substance abuse and mental health support much of the division’s programming. Funding amounts are not the same year-to-year, and the federal government could reduce funding for those grants, she said.

Often uncoordinated efforts
After her daughter, Rachel, died by suicide in 2008, Lynette Vega decided that it was important to talk about the topic and behavioral health. She received training in how to discuss suicide and worked with the Nevada Office of Suicide Prevention and other organizations to train educators to recognize warning signs and be aware of prevention strategies.
In 2020, she established Zero Suicides Elko County, a nonprofit dedicated to preventing suicide in Elko County that also serves as an advocacy and support space for families.
“Out here, of course, everybody thinks you gotta put your bootstraps on. ‘I'm OK. Nothing's wrong with me,’ kind of mentality,” Vega said. “There's not one family that you can hang a sign on outside their house that says, ‘No problems here.’ Every family's dealing with something.”


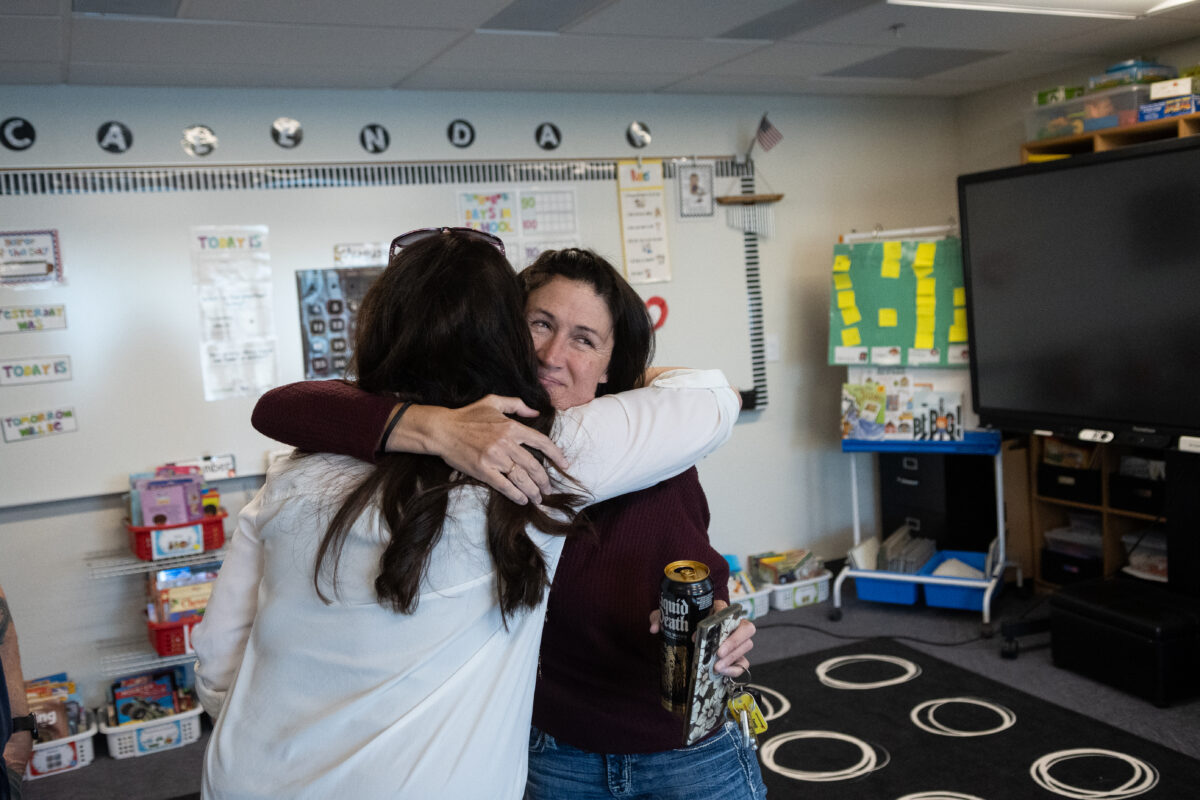
Though local efforts are vital — Denali’s mother, Maria Kauffman, said Vega’s organization was her “saving grace” after her son died — Pearce said responses to youth mental health are often isolated. This can make establishing a broader system of care challenging, she said.
The Department of Health and Human Services is the state entity responsible for coordinating services and funding in partnership with counties and other organizations. But there isn’t one specific division or entity providing or creating a broader children’s system of care.
“Because each community has unique needs and circumstances, a multi-agency effort is needed to fund and design a system that best fits each community,” officials with the department wrote in a statement.
Pearce said one solution for a unified effort would be implementing a state Office of Children’s Mental and Behavioral Health. She said the office could help disseminate information, track struggling counties, share projects that are working in other regions of the state and offer infrastructure support.
“We see the need for some type of cohesive statewide leader to guide work in this space and promote high-quality services,” Pearce said.

Ultimate care
When Jason gives presentations on health and safety, he thinks about his son and includes a discussion about mental health and how that ties to workers' safety and being fit for duty. He said Nevada Gold Mines has also launched various initiatives related to mental health and training to raise awareness.
Jason said he never shies away from reminding people that caring for yourself is important.
“It’s not something I’m afraid to admit in front of people,” he said. “We all need tuneups, just like your car needs a tuneup.”
Mosby, who oversees the NV PAL program, agreed with Jason. She said it’s essential to talk about mental and physical health, and to establish a coordinated system of care.
She said there’s often a lack of communication and collaboration between schools, health care professionals, social services and other entities involved in children’s care needs. A child might receive psychiatric care but not have their academic or social needs met, which can hinder overall progress, she said.


As of the end of November, Mosby said NV PAL had served 887 youth and 106 primary care doctors, including providing diagnostic criteria for autism and conducting more than 7,800 care coordination meetings in Spanish and English. The organization offered nearly 2,000 child and adolescent psychiatry consultation appointments with doctors, who sometimes made repeat calls about a patient’s needs.
Mosby said the program has room to grow. It’s one effort among many to help address the care gaps in Nevada, she said.
But if more progress isn’t made at an individual, local, regional or state level, Mosby warned that there could be an increase in suicide, school suspensions and other problems.
“We should be talking about ultimate care and just the holistic way of how to take care of ourselves in every system,” Mosby said.
